The 2024 Medicare PFS Final Rule and Proposed Information Blocking Disincentives

‘Regulations, Penalties, Changes, oh my!’ is what our Government Incentives team at DAS Health has been saying this past week with the Medicare PFS Final Rule Updates! On October 30, 2023 the U.S. Department of Health and Human Services (HHS) released its proposed rule on the Establishment of Disincentives for Health Care Providers that have committed Information Blocking and on November 2, 2023, the Centers for Medicare & Medicaid Services (CMS) unveiled its eagerly anticipated final rule outlining significant changes to the Medicare Physician Fee Schedule (PFS) and other Medicare Part B issues, set to take effect on or after January 1, 2024.
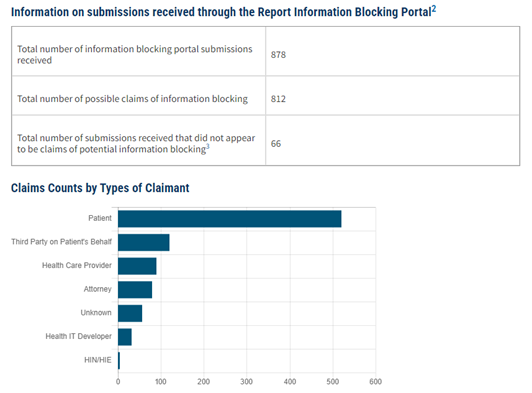
Let’s start with information blocking, HHS has proposed if an eligible clinician is found to have participated in information blocking, the clinician is not considered a meaningful user of certified EHR technology and therefor will receive a zero score in the Promoting Interoperability performance category of the Medicare Merit-based Incentive Payment System (MIPS), typically a quarter of the total MIPS score. This is currently proposed and not yet finalized, but here is a snapshot of current information blocking submissions pending investigation:
Medicare Reimbursement Adjustment
Perhaps one of the most eye-catching aspects of this final rule is the announcement of a 1.25% reduction in Medicare reimbursement for physicians in 2024. The implications of this adjustment are significant as this in addition to the Medicare sequestrations already in effect, requiring physicians to identify other sources of revenue in order to maintain a financially health practice.
Changes in the Appropriate Use Criteria (AUC) Program
Another significant change is the decision by CMS to pause the Appropriate Use Criteria (AUC) program and rescind the current AUC program regulations. This will likely come as an expected and welcomed announcement by CMS that practices no longer have to implement this functionality or be faced with claim denials.
Quality Payment Program Changes for 2024
Within the QPP, clinicians will need to adapt to several policy changes in the coming year. For those reporting under traditional MIPS in 2024, we highlighted our top ‘must know’ changes you can expect next year:
- The performance threshold will remain at 75 points for 2024, indicating a continuity in performance expectations from the previous year.
- Reporting for Promoting Interoperability will transition to a consecutive 180-day period, doubling the previous reporting period length.
- A ‘yes’ attestation for the SAFER Guide measure will be required.
- The quality measures inventory will consist of 198 quality measures, with certain measures like Breast Cancer Screening, Colorectal Screening, and BMI being removed from Traditional MIPS reporting. Similarly, Influenza and Pneumococcal vaccination measures will be eliminated from MVP reporting. There was the creation of a new measure, MIPS CQM 499 Preventive Care and Wellness, a composite measure composed of seven current preventive care and screening measures. As well as an update of the CMS 138 Tobacco measure logic to ensure the screening of all patients for tobacco use instead of just tobacco users.
For those participating in an Advanced Alternative Payment Models (APMs) starting with the 2024 performance period, all Advanced APMs must mandate the use of certified EHR technology (CEHRT). There were also updates to the QP and Partial QP determination process:
- QP and partial QP determinations will continue to be made at the APM Entity level for the 2024 performance period, rather than at the individual level.
- Notably, QP and Partial QP thresholds have been raised, requiring higher levels of participation for eligibility at both the patient and payment level.
However, the most notable APM update is that the APM incentive payment will cease after 2023, replaced by a higher Medicare conversion factor for QPs starting in 2024.
And last but not least, our newest reporting option the MIPS Value Pathways (MVPs). CMS has finalized five new MVPs, bringing the total to 16 MVPs available for reporting in the 2024 performance period. These MVPs encompass a wide range of medical specialties and focus areas, including Women’s Health, Ear, Nose, and Throat Disorders, Infectious Disorders (such as Hepatitis C and HIV), Mental Health and Substance Use Disorders, and Musculoskeletal Care.
In summary, the 2024 Medicare Physician Fee Schedule Final Rule and the accompanying changes to the Quality Payment Program represent a significant shift in the program making it more challenging to avoid a penalty and earn an incentive.
Now more than ever, clinicians must stay informed and adapt to these alterations, as they will have a direct impact on the way healthcare is delivered, measured, and compensated in the coming years. Keeping a close eye on these changes and proactively adjusting practice strategies will be essential for clinicians to thrive in this evolving healthcare landscape. And your trusted advisors at DAS Health are here to help! You can register for our complimentary educational webinar here and learn more about these changes from our team of experts. If you are interested in how our Government Incentives team can support your practice send us an email at governmentincentives@dashealth.com.